Speech pathology treatment for ILO/VCD
Using a laryngoscopy for the management of ILO/VCD
The Gold Standard for diagnosis of ILO/VCD is laryngoscopy. This can be performed with a provocation trial using the patient’s typical triggers such as odours, breathing, coughing and/or phonatory manoeuvres. If available at the clinical setting, exercise provocation may also be used. The diagnosis section of this toolkit provides further details.

Access to instrumental assessment with laryngoscopy might be challenging in some centres. In this case, a provisional diagnosis of ILO/VCD can be made based on other aspects of the clinical assessment. Functional laryngoscopy for the purpose of diagnosis of ILO/VCD is performed by a suitably trained health professional such as an otolaryngologist or speech pathologist. Laryngoscopy is necessary to rule out comorbid conditions and other medical conditions affecting the upper airway that may mimic ILO/VCD. The differential diagnosis is essential before evidence-supported behavioural intervention is initiated. If a speech pathologist is involved in the diagnostic process, some components of treatment may be delivered as part of the clinical assessment.
If the treating speech pathologist has not been involved in the diagnosis of ILO/VCD they should have a thorough understanding of the patient’s medical history and presentation of the condition for diagnosis of ILO/VCD prior to commencing therapy. It is also important for the speech pathologist to understand what formal testing has been used to confirm the ILO/VCD diagnosis and that relevant co-morbidities have been identified and other medical conditions as the primary cause of the breathlessness have been excluded.
Patients need to be examined by a pulmonary specialist to confirm or rule out a component of asthma. If the patient presents with co-morbid asthma, confirming the diagnosis and optimising treatment of asthma by a respiratory specialist for the individual patient should be prioritised.
Showing patients the video of their own laryngoscopy (with or without provocation) before commencing treatment can help them understand the nature of their condition, the rationale for treatment, improve interoception of laryngeal posture for breathing and facilitate treatment adherence. If this is not possible e.g. if the laryngoscopy was not recorded, then showing a publicly available video of a patient with ILO/VCD can be helpful with an explanation of similarities or differences to that person’s individual ILO/VCD profile.
Treatment should be provided by a speech pathologist with experience in treating upper airway disorders or with the support/supervision of a speech pathologist experienced in this area.
The overarching aim of speech pathology treatment is to reduce inappropriate laryngeal narrowing during respiration and to address any breathing pattern disorder if present.
Components of treatment include:
Informational education and orientation
Such as basic anatomy / physiology of breathing; rationale for therapy; difference between appropriate breathing patterns, and maladaptive laryngeal postures and respiratory patterns; differences between asthma and ILO/VCD mechanics, symptoms and treatment; and role of the larynx in the prevention and triggering of symptoms.
Reduction of laryngeal irritation and hyper-responsiveness
For example identify and manage triggers, optimise vocal health, and elimination or reduction of potential contributors such as laryngopharyngeal reflux.
Laryngeal and respiratory retraining and symptom control
Including increased interoception (the awareness of internal sensations) in the body of appropriate respiratory patterns, strategies to increase voluntary control over inappropriate laryngeal narrowing and vocal fold position during respiration, and development of appropriate thoracic and abdominal breathing control. Techniques may include sniff, abdominal breathing, the Olin exercise or inspiratory muscle training.
Support and affective counselling
This can help address the impact of ILO/VCD on a person’s overall quality of life and wellbeing.
Laryngeal imaging and biofeedback
The speech pathologist may use the laryngoscopy examination for biofeedback and to test stimulability for treatment techniques during laryngoscopy. This examination may also later serve as a therapy tool for education of the nature of the condition and for increased patient interoception.
Behavioural management for comorbid symptoms
Hoarseness and cough are common comorbidities. These should be identified through the assessment process. The behavioural management plan should take these into account.
Treatment
A clear understanding of the nature of the condition, provision of ILO/VCD episode prevention and rescue strategies and the rationale for specific exercises are critical to treatment success.
Exercises need to be nuanced to the individual ILO/VCD profile of the patient with due consideration of the desired outcome. In general however such exercises involve laryngeal postures that promote vocal fold abduction and/or optimal laryngeal aperture dimension for respiration (e.g., sniff/nasal breathing, pursed lips or fronted tongue posture to achieve oral or lingual resistance, abdominal focus of breathing etc.) Typically patients require repeated opportunity to practice in and outside of the therapy session, in order to perform therapy techniques competently with confidence and before being able to transfer these skills and implement techniques to control their symptoms external to the clinical context. The speech pathologist provides supervision and feedback to the patient when performing exercises.
Exercises may not be as effective for many patients without also providing sufficient training, opportunities for supervised practice and evaluation of accuracy of execution. Competency in practice maybe more difficult to achieve for patients e.g. those with exercise induced laryngeal obstruction (EILO) or concomitant respiratory disease. Treatment for EILO is covered separately in this Toolkit.
Gentle provocation of symptoms during treatment sessions can be helpful to allow patients to experience success in using treatment techniques to control symptoms.
Treatment progress and evaluation
Progress should be regularly monitored using standardised patient-reported outcome measures in order to capture the patient experience and determine congruence with clinician and healthcare utilisation measures of change. The VCD-Q and EILODI are specifically designed and validated to measure treatment progress, though in clinical practice the instruments used are variable.
Some examples are below:

It may also be necessary to address comorbid symptoms such as evaluation and treatment of Gastro-oesophageal Reflux Disease (GORD) in patients with GORD symptoms, globus, cough and dysphonia if these are present and to mitigate any laryngopharyngeal reflux or nasal obstruction contributions as required.
It is also important to communicate clinician-predicted prognosis and treatment outcomes to the patient and the multidisciplinary team. It is generally helpful to report on patient immediate stimulability for changed laryngeal postures and subjective and objective measures of improvement over time, and aspects of the patient’s adherence to treatment including attendance at appointments, perceived understanding of the rationale for laryngeal and respiratory retraining, home practice of provided exercises, accuracy with techniques, and reported implementation of strategies.
Evaluation of condition responsiveness and overall therapy effectiveness will generally be a combination of:

Although there is little data on the recommended speech pathology treatment dose (i.e. the number and spacing of therapy sessions and frequency and duration of home practice), in keeping with motor learning principles, it is assumed that more frequent practice and integration into daily routines is likely to be associated with improved outcomes. Experienced clinicians observe that good outcomes are achieved within 2-4 sessions but patients may subsequently require regular reviews over a 1-2 year period to maintain improvement. Patients need to commit to daily practice of respiratory exercises as part of their therapy program.
Service delivery models can vary according to patient and clinician needs and context. Some patients may require frequent sessions in order to master the therapy techniques before they can then apply and graduate these into different contexts and intensities. Other patients may require less therapy sessions or ones spaced further apart, to provide sufficient time to practice the respiratory exercises, to develop muscle memory and become proficient in respiratory control before introducing more advanced exercises.
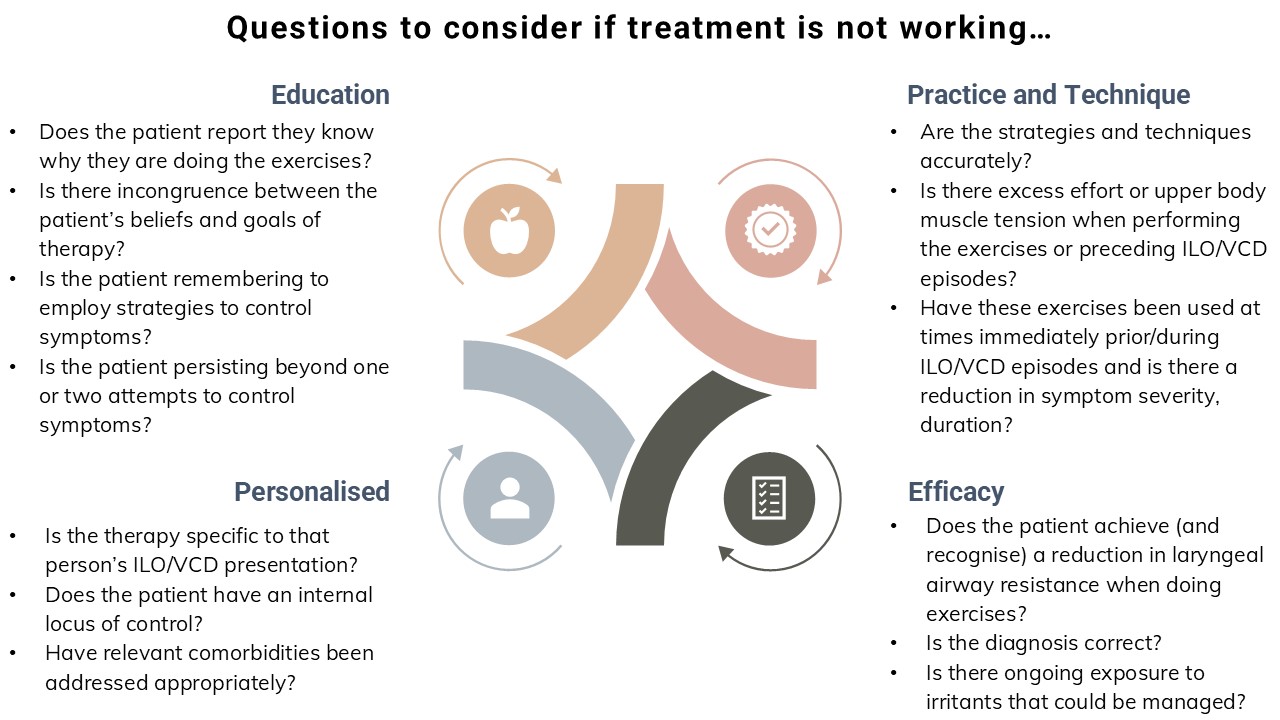
Troubleshooting
Therapy outcomes are often affected by patient engagement in the therapeutic process. Ensuring the patient has a clear understanding of the rationales for the laryngeal and respiratory retraining and the inherent underlying functional changes achieved by the exercises and strategies is an important consideration. Speech pathologists may need to revisit their explanations and consider different approaches to the implementation of exercises and strategies to improve patient engagement and thereby optimise outcomes.